The incidence of type 1 diabetes is placing an increasing burden on the healthcare system. With the aim to improve outcomes for people with diabetes (i.e. fewer hospitalisations by fewer complications and better quality of life) and contain costs, Dr Henk Veeze and Dr Henk-Jan Aanstoot founded Diabeter in 2006 in the Netherlands. It is now a Dutch-certified clinic with more than 2000 people with diabetes in 5 locations, specializing in providing comprehensive and individualized care for children and adolescents with type 1 diabetes. They are pioneering diabetes care, founded on value-based e-health solutions and a unique care experience.
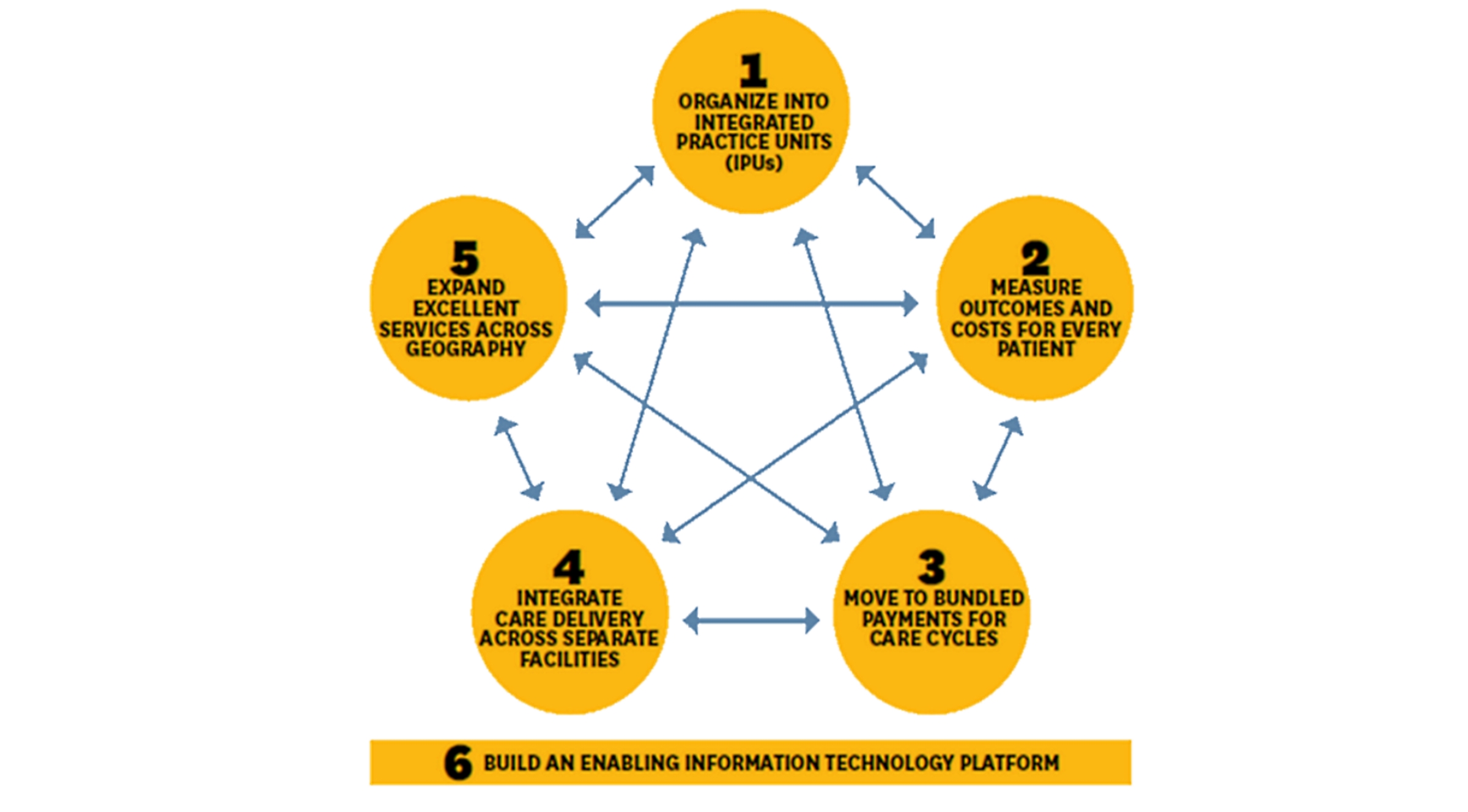
Their concept resembles the value-based healthcare (VBHC) model as put forward by Professor Porter of Harvard Business school. He stressed the need for transforming healthcare systems by improving the value of healthcare for people with diabetes without raising costs and/or maintain high-standard care at lower costs. VBHC is based on 5 pivotal pillars: 1) Integrated practice units (IPU: healthcare providers organized around the medical condition of the person with diabetes; 2) Measuring outcomes and costs of the entire care cycle, and improve value; 3) Bundled payment for care cycles, to prevent volume over quality; 4) Integrate care delivery (dedicated facilities); 5) Expansion across regions. These should be interconnected by information and communications technology (ICT) platforms for data collection, decision support and coupling technology with big data and analytics.
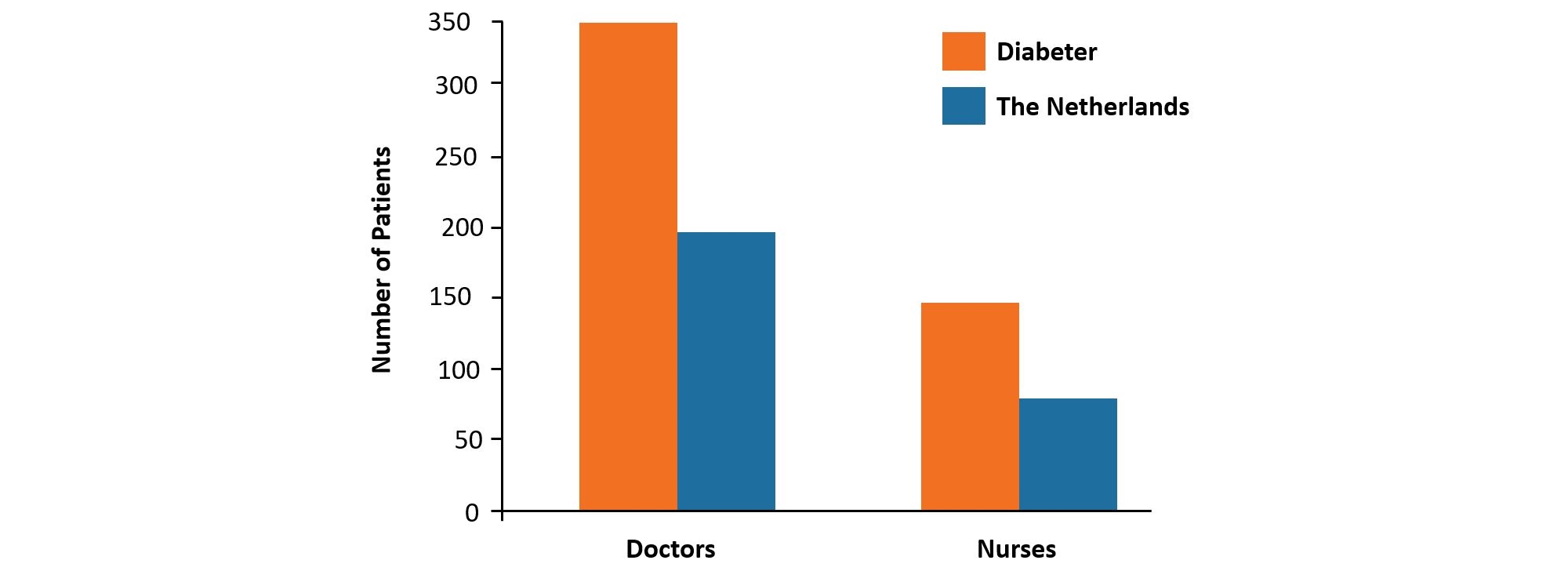
Diabeter operates outside of the traditional hospital setting and with dedicated personnel (medical doctors, nurses, dieticians, psychologists, administrative staff). As type 1 diabetes is a chronic disease, the practised care cycle is geared towards intensifying contacts between the person with diabetes and healthcare provider (visits, phone, e-mail, Skype), leading to more active participation of the person with diabetes. Each person with diabetes has a care manager who is responsible for the entire care cycle and contact person for all concerned (i.e. people with diabetes and care givers). ICT is indispensable: using VCare, a custom-built patient record system, data from glucose meters and/or insulin pumps can automatically be uploaded, allowing people with diabetes to monitor their own data in real-time on a dashboard. Vcare provides care managers with e-mails on status of the person with diabetes and after analysis, they receive a ‘Ther@py mail’ with info on trends, target setting, treatment plans and follow-up appointments. In case of large deviations in the data, automatic alerts are sent to the treating physician.
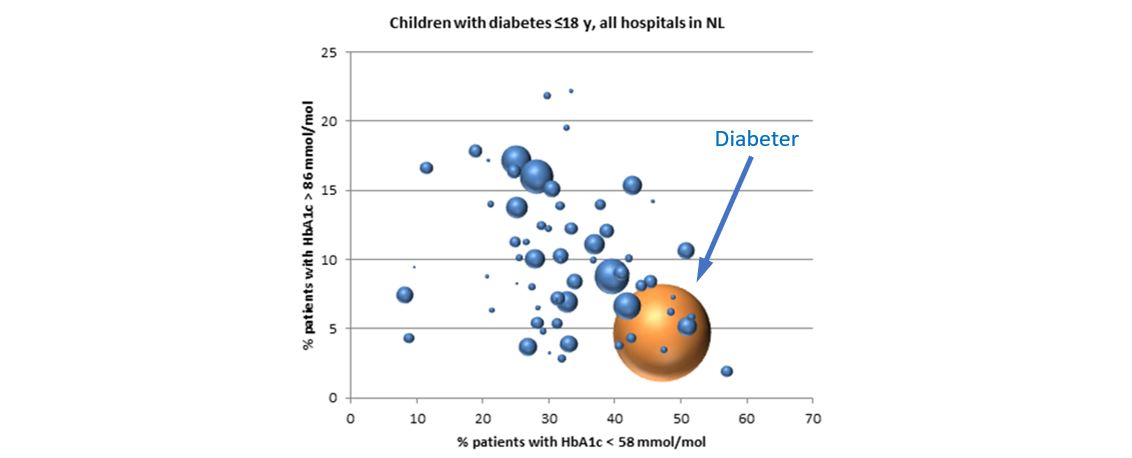
Outcomes in 3 categories are continuously monitored (health status achieved, care process and complications, sustainability of health), as well as costs. More than half of people with diabetes at Diabeter are at target (55% of children < 18 years reach HbA1c < 7.5% [58 mmol/mol]) and fewer are hospitalized (1-3%) compared with most other clinics (10%), with yearly costs staying constant (65-70% personnel; remainder for laboratory tests, admin, IT, accounting, marketing and rent).
Summarizing, using value-based solutions, Diabeter is shifting from spending on acute interventions to improving chronic disease management, with people with diabetes enjoying greater freedom and better health. Please find our white paper here.